
In the world of medical anomalies, some conditions stand out as fascinating puzzles that challenge our understanding of the human body. One such enigmatic condition is Ludwig’s Angina, a rare and potentially life-threatening infection that affects the floor of the mouth and neck. Named after the German physician Wilhelm Friedrich von Ludwig who first described it in the 19th century, this ailment offers a unique glimpse into the complex interplay of anatomy, microbiology, and clinical expertise.
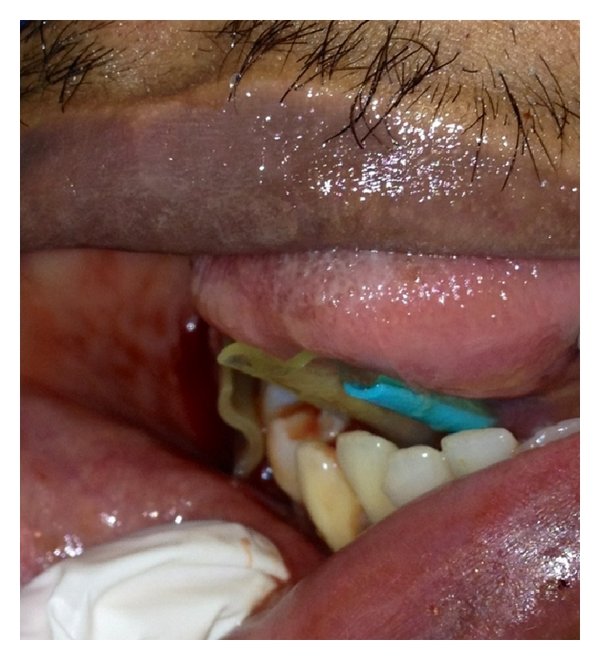
Ludwig’s Angina primarily develops as a result of an infection in the roots of the teeth, often stemming from untreated dental infections or abscesses. The infection rapidly spreads through the soft tissues of the floor of the mouth and neck, leading to painful swelling, difficulty in swallowing, and even airway obstruction. Although advancements in dental hygiene and medical care have made cases of Ludwig’s Angina relatively rare, it remains a stark reminder of the intricate connections between oral health and overall well-being.

The key to managing Ludwig’s Angina lies in its prompt diagnosis and aggressive treatment. Antibiotics are administered to combat the bacterial infection, while surgical intervention might be necessary to drain abscesses and alleviate airway obstruction. The collaborative efforts of dentists, oral surgeons, and infectious disease specialists are crucial in tackling this condition effectively.
Managing Ludwig’s Angina surgically requires a multi-faceted approach aimed at promptly relieving the airway obstruction, draining the abscesses, and addressing the underlying infection. Here’s a more detailed look at the surgical management of Ludwig’s Angina:
1. Airway Management: In severe cases of Ludwig’s Angina where there is a risk of airway obstruction due to swelling, establishing a secure airway takes precedence. This can be achieved through procedures such as orotracheal intubation or tracheoatomy/cricothyroidotomy. Airway management is often the first step to ensure the patient’s survival before proceeding with other surgical interventions.


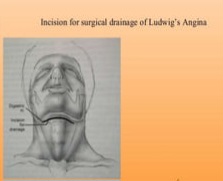
2. Incision and Drainage: Once the airway is secure, the next step is to drain the infected areas and reduce the swelling. Surgical drainage of the affected regions is crucial to alleviate the pressure and prevent the further spread of infection.
This involves making incisions in the floor of the mouth and neck to allow pus and fluid to drain out. Here’s a more detailed breakdown of the incision and drainage process:
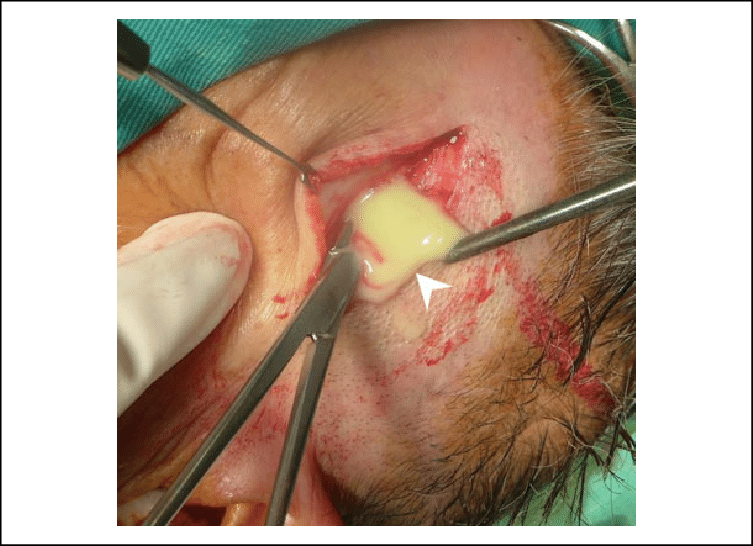
a) Identifying Swollen Areas: The surgeon assesses the patient’s condition to determine the locations of maximum swelling and tenderness. These areas typically correspond to the points of greatest infection and abscess formation.
b) Choosing Incision Sites: The surgeon selects optimal sites for incisions that provide access to the infected areas and allow for effective drainage. Incisions are typically made on the floor of the mouth, below the tongue, and in the neck region, targeting the areas where the infection has spread.
c) Types of Incisions: The choice of incisions can vary based on the surgeon’s preference and the specific anatomy of the patient. Commonly used incisions include sublingual incisions, submental incisions, and cervical incisions. Sublingual incisions are made under the tongue, submental incisions are located just below the chin, and cervical incisions are made in the neck region.
d) Drainage of Abscesses: Once the incisions are made, the surgeon carefully dissects through the layers of tissue to reach the abscesses. The pus and infected material are gently drained out, relieving pressure on surrounding tissues. If multiple abscesses are present, additional incisions may be made as needed.
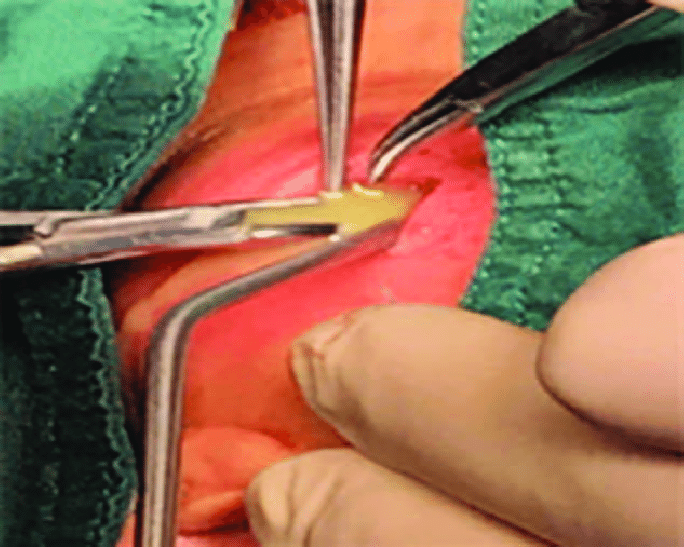
e) Irrigation and Debridement: The surgical area is irrigated with sterile saline solution to flush out remaining debris and bacteria. Any necrotic (dead) tissue is carefully removed (debrided) to prevent further infection and encourage healthy tissue healing.

f) Placement of Drains: In some cases, surgical drains may be inserted into the incision sites to help facilitate ongoing drainage of fluid and prevent the accumulation of pus (passive open drain e.g. corrugated/penrose). These drains are typically left in place temporarily and are removed once the drainage decreases and the infection is under control.

g) Closure: Depending on the extent of the incisions and the surgeon’s preference, the incisions may be closed partially or left open to allow for continued drainage. Sutures or wound closure techniques that minimize tension on the wound are used to ensure optimal healing.
f) Surgical samples management: The sample of the pus and abscess wall collected after the incision and drainage procedure is sent for investigations, including culture and sensitivity, tuberculosis workup, and histopathology.
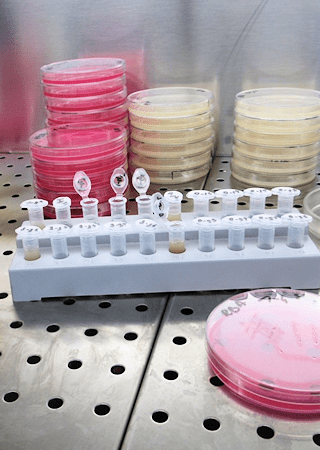
3. Control of Infection: Samples of the infected tissue may be sent for cultures to identify the causative bacteria. This information helps guide the choice of antibiotics for effective infection control. Intravenous antibiotics are typically administered to target the specific bacteria causing the infection. Typically, antibiotics are used in combination to provide coverage for both aerobic and anaerobic bacteria. For instance, a broad-spectrum antibiotic like coamoxiclav or a cephalosporin is often paired with metronidazole.
4. Collaborative Approach: Managing Ludwig’s Angina often requires a collaborative effort between oral and maxillofacial surgeons, otolaryngologists, and infectious disease experts. This interdisciplinary approach ensures comprehensive and effective treatment of the condition.

5. Wound Care and Follow-up: After surgical drainage and infection control, wound care becomes essential for proper healing. Patients may require regular follow-up appointments to monitor their progress and ensure that the infection is fully resolved. Proper wound care instructions, along with any necessary medication, are provided to the patient for home management.

6. Monitoring and Complications: Patients recovering from Ludwig’s Angina surgery need to be closely monitored for any signs of recurrent infection, delayed healing, or complications. Swelling, difficulty in swallowing, and pain should be carefully observed and managed.

Surgical intervention for Ludwig’s Angina is reserved for cases that are severe, rapidly progressing, or those that do not respond to conservative treatments like antibiotics. The timing of surgery is critical, as prompt intervention can significantly improve outcomes and reduce the risk of life-threatening complications.
What makes Ludwig’s Angina all the more intriguing is its capacity to test medical professionals’ diagnostic acumen. Its presentation can mimic other conditions, such as deep neck infections or allergic reactions, adding an element of challenge to the diagnostic process. Quick and accurate identification is paramount, as a delay in treatment can lead to complications like sepsis or even death.

In conclusion, Ludwig’s Angina stands as a captivating example of the intricate web of health and disease. Its rarity and potential severity demand our attention, urging us to remain vigilant about dental hygiene and prompt medical care. The lessons we glean from understanding and managing this condition reverberate throughout the broader medical landscape, reminding us of the ongoing pursuit of knowledge that underpins the practice of medicine.






























Leave a comment