While pulmonary tuberculosis often dominates global health discussions, Tuberculous (TB) lymphadenitis remains the most prevalent form of extrapulmonary tuberculosis (EPTB).
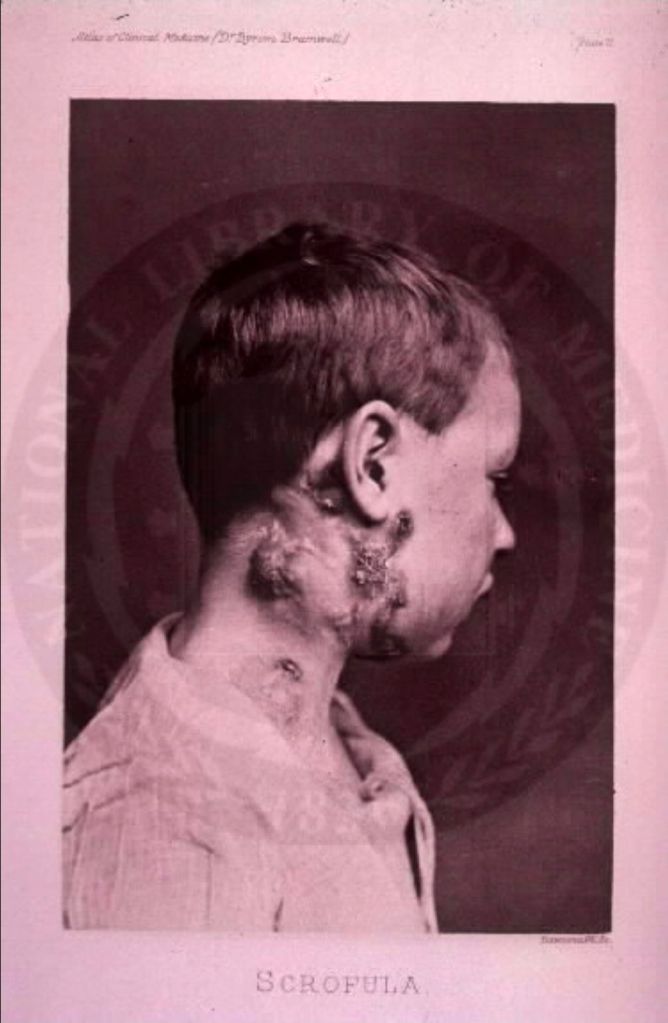
Often presenting as a painless, “cold” swelling in the neck, its indolent nature frequently leads to diagnostic delays. However, evidence-based findings from renowned journals like The Lancet and The Journal of Infection in Developing Countries highlight that this “silent” infection is far from harmless.

1. The Progression to “Collar-Stud” Abscesses
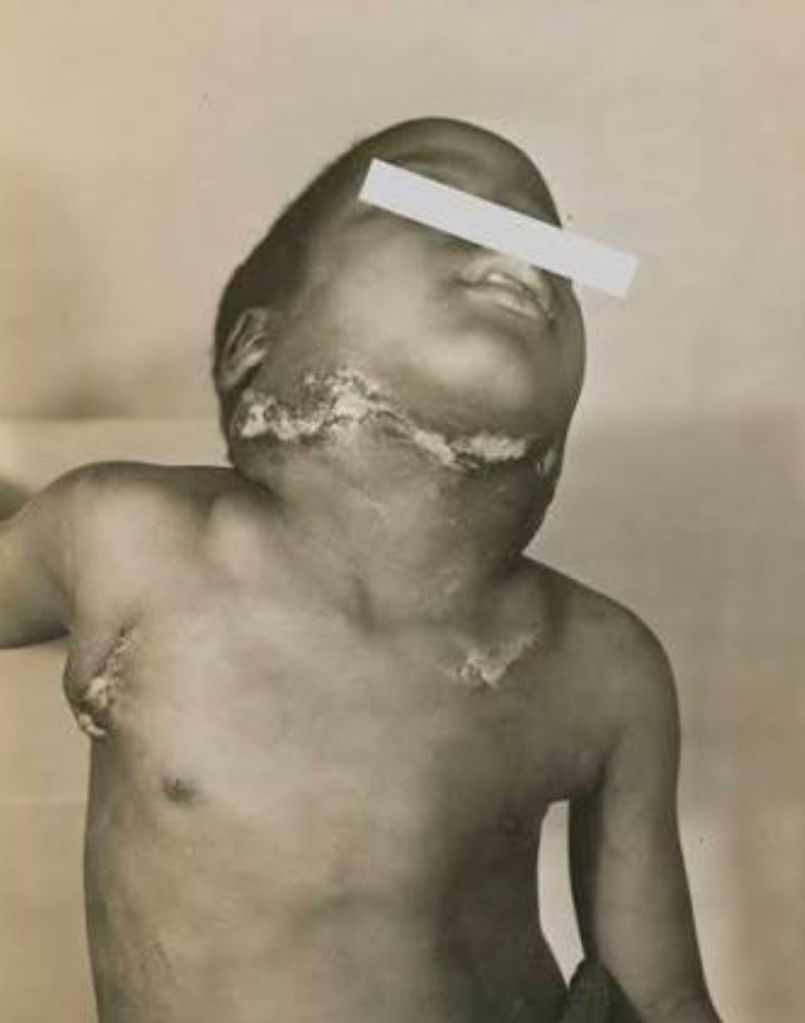
One of the primary dangers of untreated TB lymphadenitis is the predictable yet destructive progression of the lymph node.
Clinical studies categorize the disease into five distinct stages. Without intervention, the infection moves from simple enlargement to caseous necrosis—a process where the center of the lymph node turns into a soft, cheese-like substance.
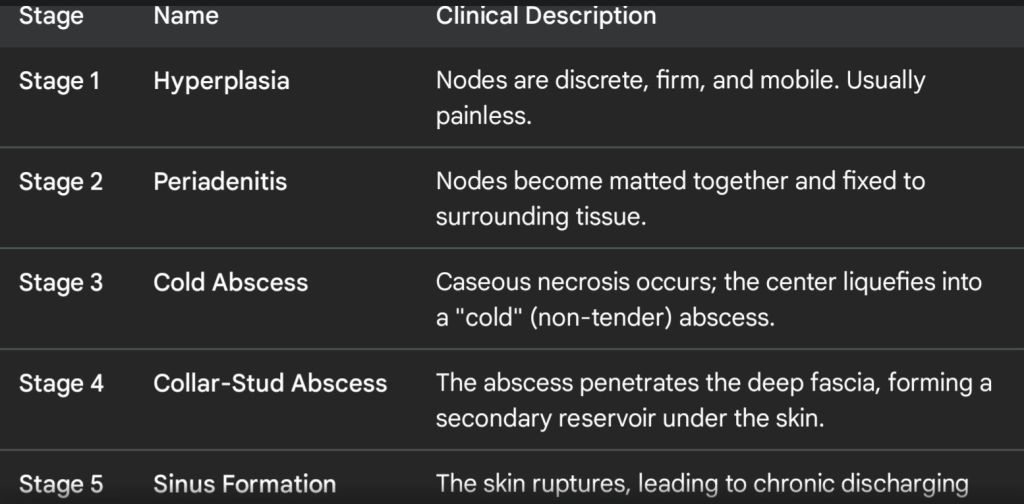
This leads to the formation of a “collar-stud” abscess, where the infection perforates the deep fascia and accumulates under the skin. If the pressure continues, it ruptures, creating chronic discharging sinus tracts. These tracts are notoriously difficult to heal and often result in permanent, disfiguring scars.

2. Systemic Hematogenous Dissemination
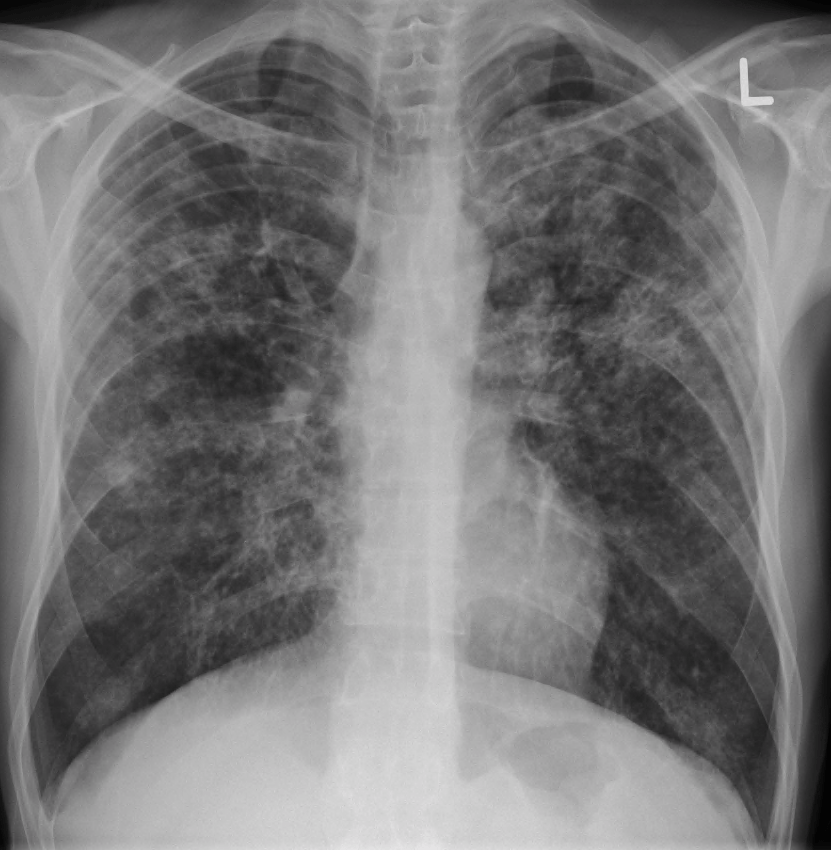
Though TB lymphadenitis is often localized to the cervical (neck) nodes, medical journals emphasize that it is a local manifestation of a systemic disease. The Mycobacterium tuberculosis bacilli can travel through the lymphatic system or the bloodstream.
a) Miliary Tuberculosis: In immunocompromised individuals or those with high bacterial loads, the infection can disseminate throughout the body, affecting the marrow, liver, and spleen.
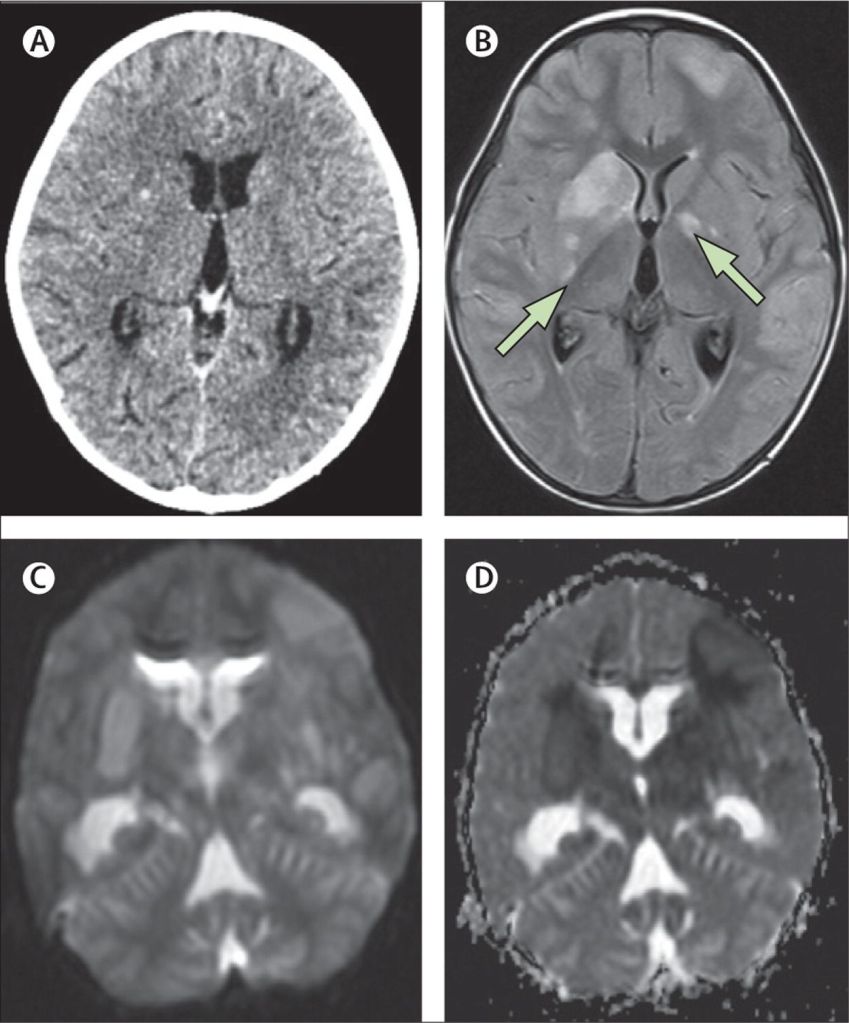
b) TB Meningitis: Evidence suggests that EPTB can seed the central nervous system, leading to life-threatening inflammation of the brain membranes.
3. Compression of Vital Structures
As lymph nodes enlarge (lymphadenopathy), they can exert mechanical pressure on surrounding anatomical structures. Research published in PMC reports cases where massive mediastinal or cervical nodes have led to:
1- Dysphagia: Difficulty swallowing due to esophageal compression.
2- Hoarseness: Damage or pressure on the recurrent laryngeal nerve.
3- Airway Compromise: In rare, severe cases, enlarged nodes can obstruct the trachea, particularly in pediatric patients.
4. The Diagnostic Trap: Mimicking Malignancy
The “danger” of TB lymphadenitis is also diagnostic. Because it mimics lymphoma or metastatic carcinoma, a misdiagnosis can lead to inappropriate surgeries or delayed cancer treatment.
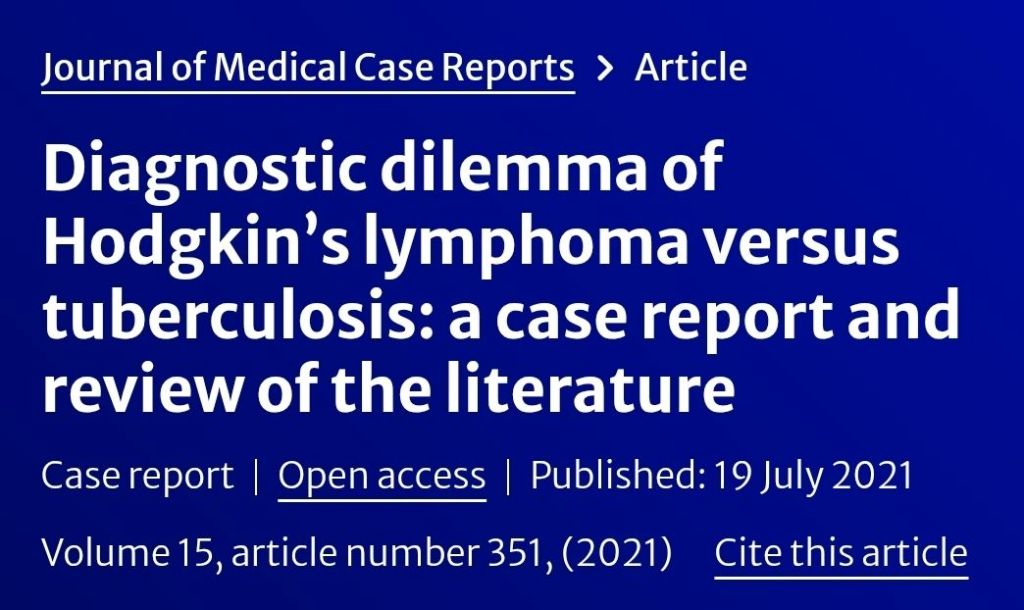
Conversely, treating a patient for a simple bacterial infection with standard antibiotics (which do not kill TB bacilli) allows the M. tuberculosis to develop drug resistance, making eventual treatment significantly more complex and toxic.
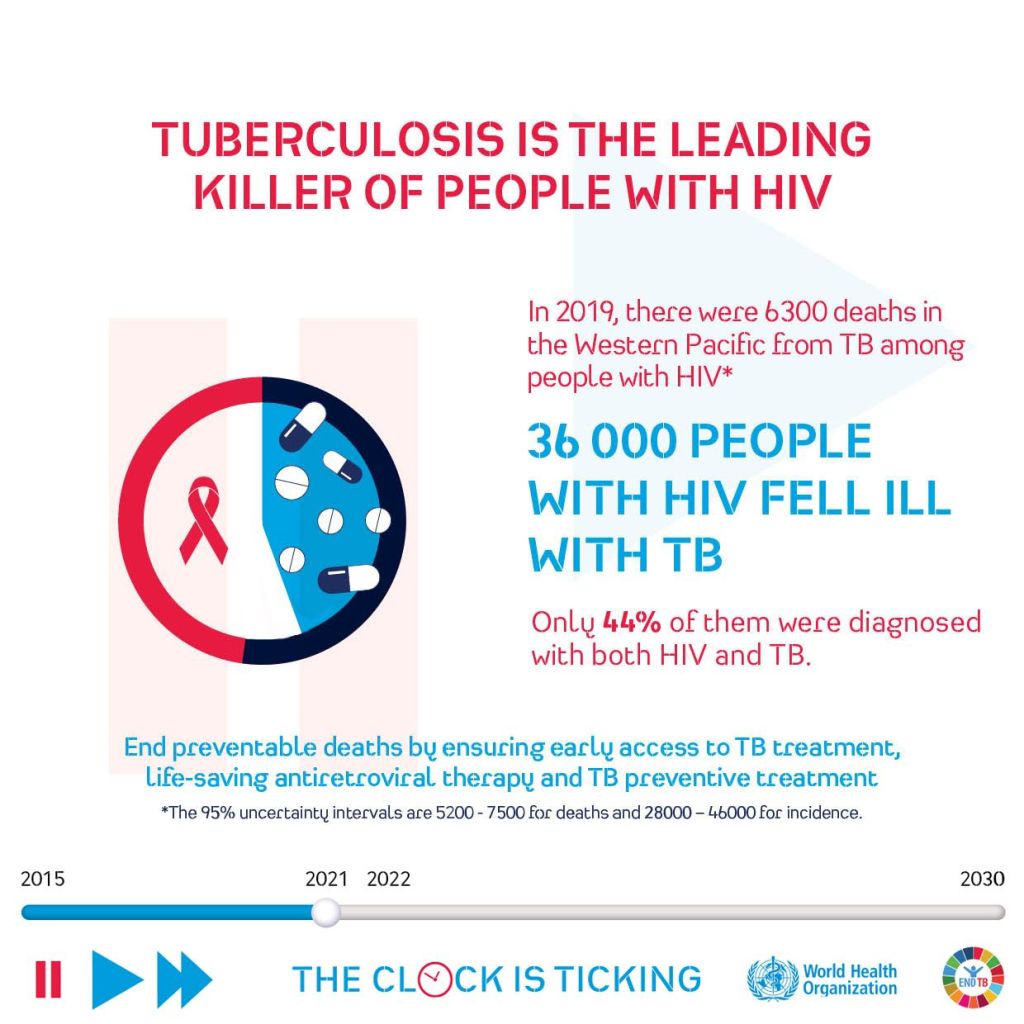
5. Comorbidity and Immune Risks
Clinical data shows a high correlation between TB lymphadenitis and HIV/AIDS. In these patients, the disease progresses more aggressively and may present as Immune Reconstitution Inflammatory Syndrome (IRIS) once antiretroviral therapy begins. This paradoxically worsens the inflammation, increasing the risk of organ failure or severe systemic distress.
6. Is Neck TB dangerous?
Neck tuberculosis (TB), also called tuberculous lymphadenitis, can be dangerous if left untreated, but it is highly treatable when diagnosed early. The infection usually affects the lymph nodes in the neck and may cause painless swelling, fever, night sweats, or weight loss. If ignored, the swelling can enlarge, form abscesses, or create chronic discharging sinuses, leading to scarring and prolonged infection. In rare cases, TB can spread to the lungs or other organs. The good news is that with proper anti-TB medication and specialist care, most patients recover fully without long-term complications. Early medical assessment is key.
Conclusion
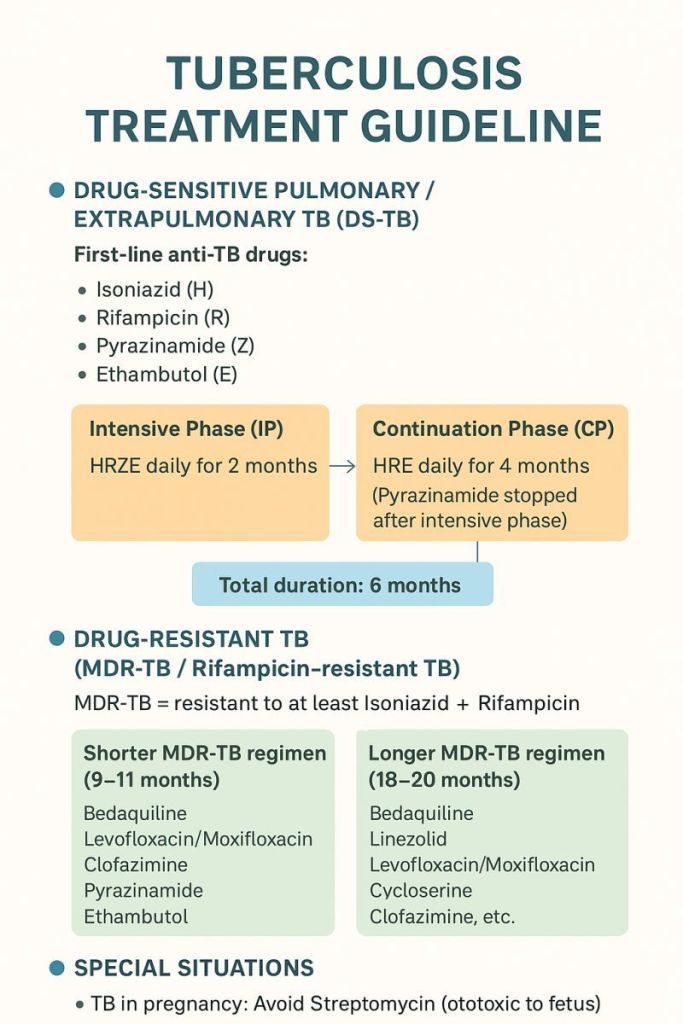
TB lymphadenitis is not merely a “swollen gland.” It is a complex infectious challenge that requires a high index of suspicion, Fine Needle Aspiration (FNA), and a strict 6-to-9-month regimen of anti-tubercular therapy (ATT). Early detection is the only definitive way to prevent the disfigurement of sinus tracts and the lethal risks of systemic spread.































Leave a comment