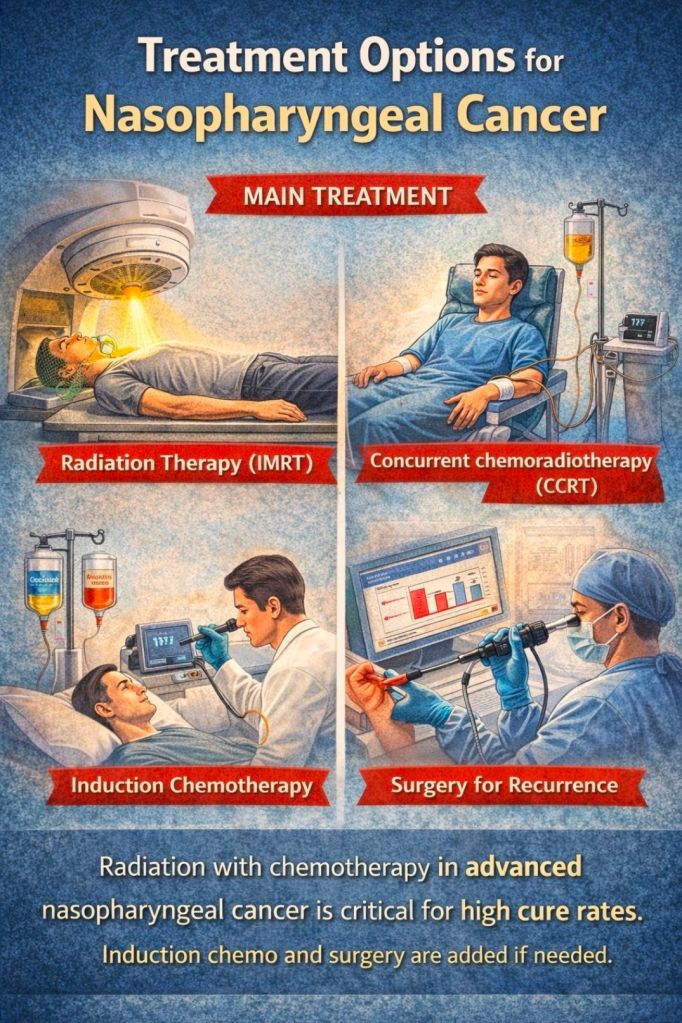
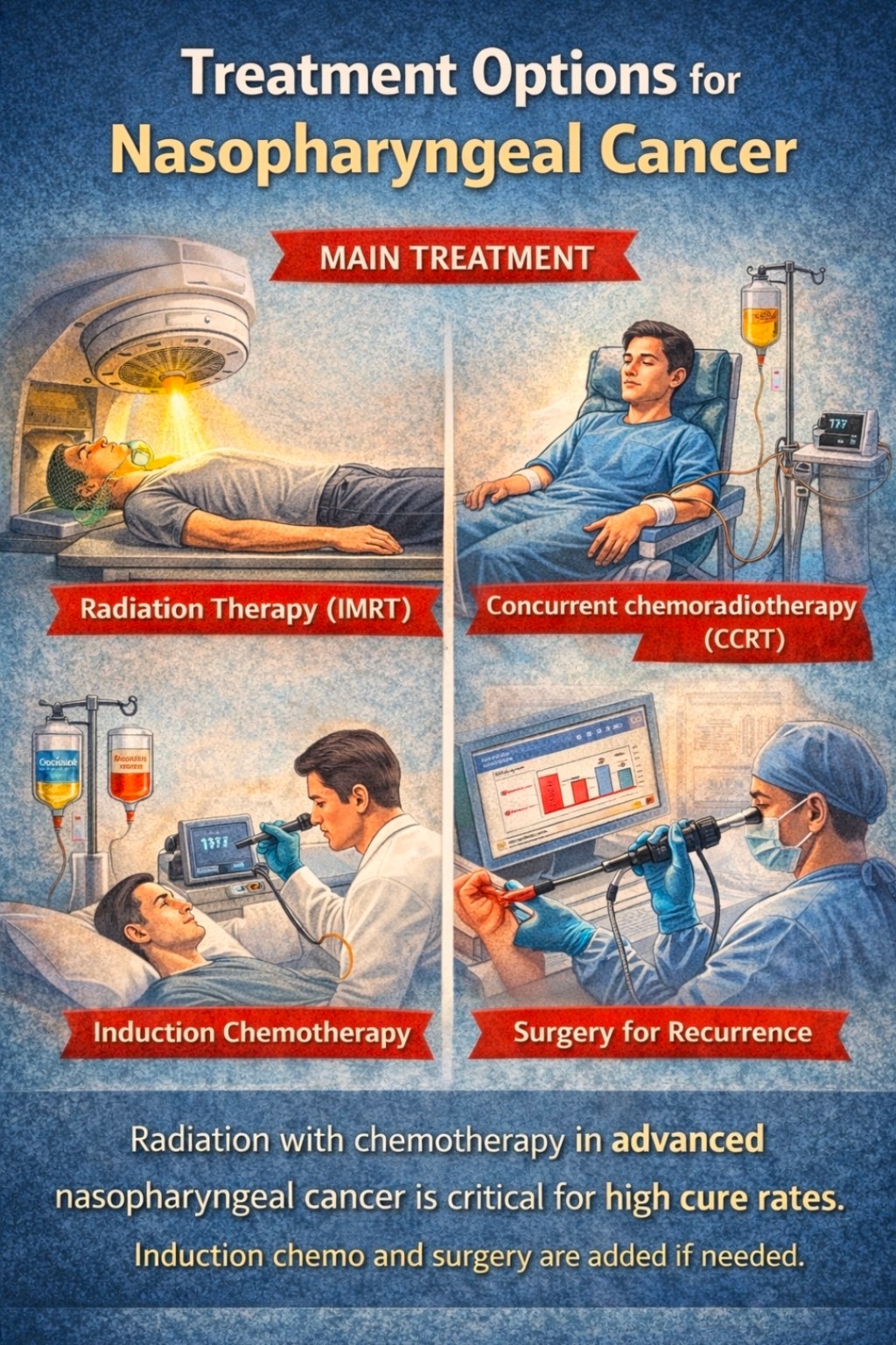
Part 5: Treatment Options
So how do we fight NPC? The frontline weapon is radiotherapy. Historically, NPC was one of the first cancers shown to be very radiosensitive. Today, every newly diagnosed NPC (even Stage I) gets high-dose radiation to the nasopharynx and neck. We cover both sides of the neck because microscopic disease can lurk in the lymph nodes even if they look normal on scan.

In the past decade, Intensity-Modulated Radiation Therapy (IMRT) has been a game-changer. IMRT allows doctors to “mold” the radiation beams exactly to the tumor’s shape, sparing nearby organs like the brainstem, spinal cord, and salivary glands. Studies show that centers using IMRT achieve excellent tumor control – local control rates and 5-year survival well above 80%.
By contrast, older 2D techniques gave far worse outcomes. For example, Malaysian hospitals without IMRT reported 5-year survival around 33–38% in the early 2000s; after adding concurrent chemotherapy it improved to ~50–58%. But once IMRT was routinely used, top centers saw 5-year survival jump to 80% or more. That’s a testament to how precision radiation can tame NPC.

Radiation does have side effects. Patients often experience fatigue during treatment, and long-term they can have hearing loss (from inner ear exposure) and endocrine changes if the pituitary gets some dose. Our goal is always to shrink radiation fields where possible, but trade-offs exist: you have to give enough dose to kill cancer.
Even so, IMRT has dramatically reduced complications compared to historical techniques. Specialists (ENT surgeons, radiation oncologists, medical oncologists) work as a team to balance treatment efficacy against quality of life.

For advanced NPC (Stage III-IV), we almost always add chemotherapy. There are two main strategies: Concurrent chemoradiotherapy (CCRT), where high-dose cisplatin (or a similar drug) is given on the same schedule as radiation; and Induction chemotherapy before radiation. CCRT became the standard after trials showed it improved control compared to radiation alone. The chemo acts like a sensitizer and also treats micrometastases.

Commonly, we give cisplatin every three weeks during radiotherapy. Induction chemo (usually 2–3 cycles of cisplatin plus gemcitabine or docetaxel-based regimens) is used to shrink bulky tumors first. Recent evidence supports induction: a large trial showed induction plus CCRT gave better survival than CCRT alone in high-risk NPC (this trial wasn’t easily accessible here, but it’s well-known).
Interestingly, a 2023 Chinese trial asked whether we truly need concurrent chemo after induction. The result was surprising: in patients who all received induction chemo, adding concurrent cisplatin during radiation did not significantly change 3-year progression-free survival. In fact, 3-year PFS was ~76% whether or not concurrent chemo was given. This suggests that for some patients, radiation alone after induction might be enough – sparing them the extra toxicity of chemo. It’s like using a two-stage attack: if the initial bombardment (induction) has already crippled the enemy, maybe you don’t need the artillery barrage (concurrent chemo) on top. These findings are still fresh, but they highlight how NPC therapy is evolving.

Surgery is rarely first-line for NPC, because the tumor is so deep. However, it has a role in salvage situations. If a patient develops residual or recurrent disease in the neck nodes after radiation, a surgeon can remove them (neck dissection). For local recurrences in the nasopharynx, advanced endoscopic techniques are now possible. Skilled surgeons in big centers can even do an endoscopic nasopharyngectomy – essentially, accessing the nasopharynx through the nose or sinuses to remove a recurrent tumor. These procedures are complex (the tumors sit near the skull base), but they’ve shown success when done in specialist centers. Think of surgery as the “Hail Mary” play: it’s not the first game plan, but when the usual treatments can’t fully eliminate the cancer, a well-placed strike by a surgeon can score a win.

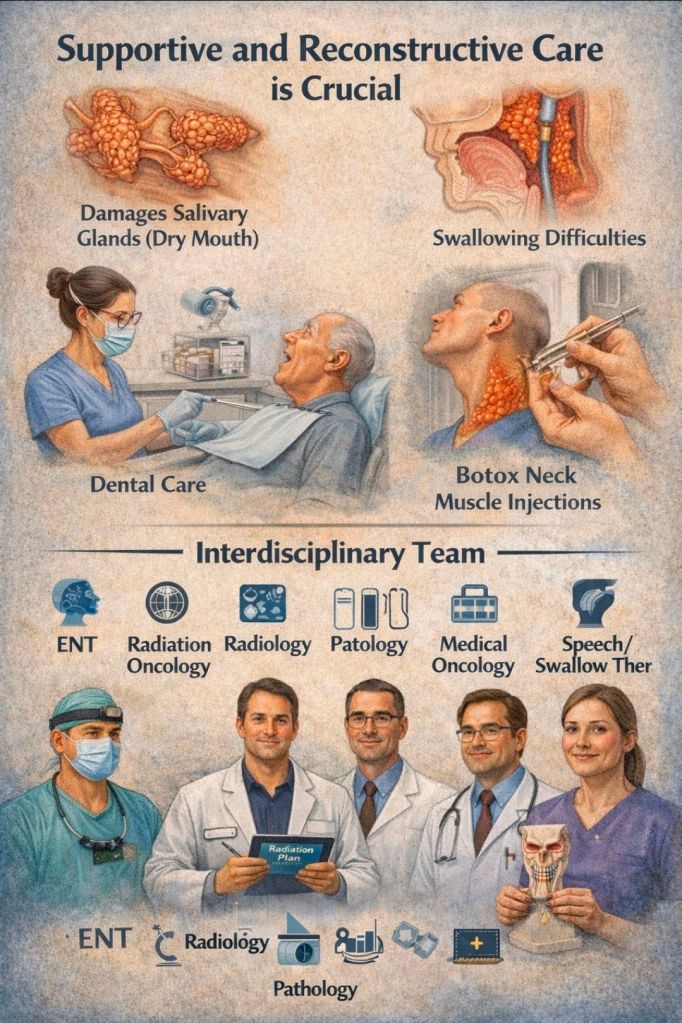
Finally, supportive and reconstructive care is crucial. Radiation often damages salivary glands (causing dry mouth) and sometimes swallowing muscles. Patients may need dental care, swallowing rehab, or injections of Botox to reduce neck muscle tightness. An interdisciplinary team – ENT, radiation, medical oncology, radiology, pathology, plus speech/swallow therapists – is essential. As one expert put it, treating NPC is a team effort. We’re all in the bunker together, coordinating rounds of chemo and radiation to win this fight.































Leave a comment