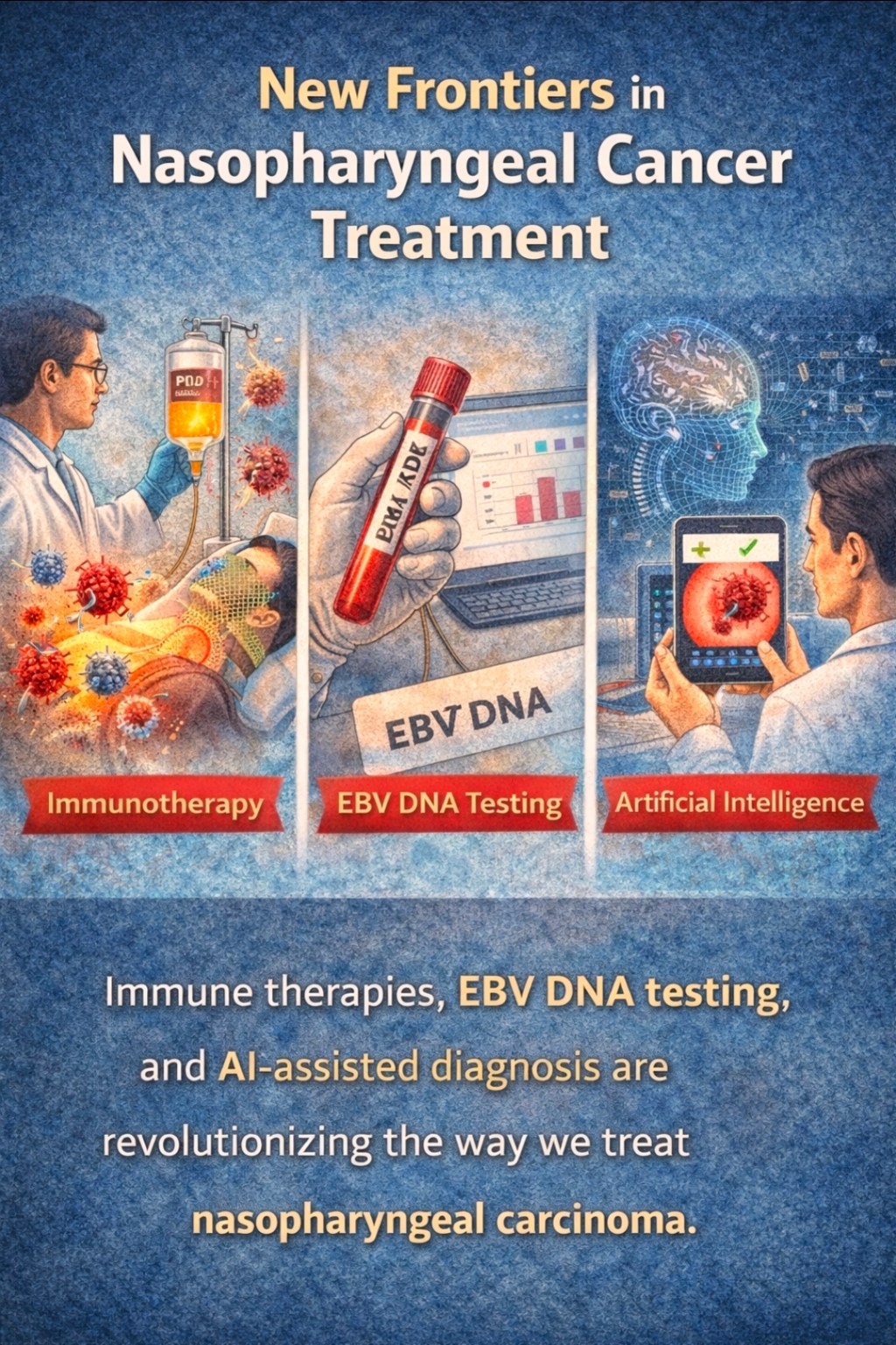
Part 6: Emerging Therapies and Research Frontiers
Exciting advances are on the horizon for NPC. One hot area is immunotherapy – treatments that harness your own immune system to fight cancer. Since NPC is driven by a virus (EBV), it’s a natural target for immune approaches. The most clinical success so far has been with PD-1/PD-L1 checkpoint inhibitors. These drugs (like pembrolizumab and nivolumab) take the brakes off immune T cells. In recent years, Chinese regulators have approved anti-PD-1 drugs specifically for NPC: toripalimab and camrelizumab. These agents showed benefit in recurrent or metastatic NPC after other treatments failed. For example, toripalimab plus chemo became a new standard for first-line metastatic NPC based on large trials (the details are beyond our quick survey). The bottom line: anti-PD-1 therapy is now part of the arsenal for advanced NPC in Asia. It’s like giving the patient’s immune system a new weapon – one that recognizes and kills EBV-infected tumor cells.
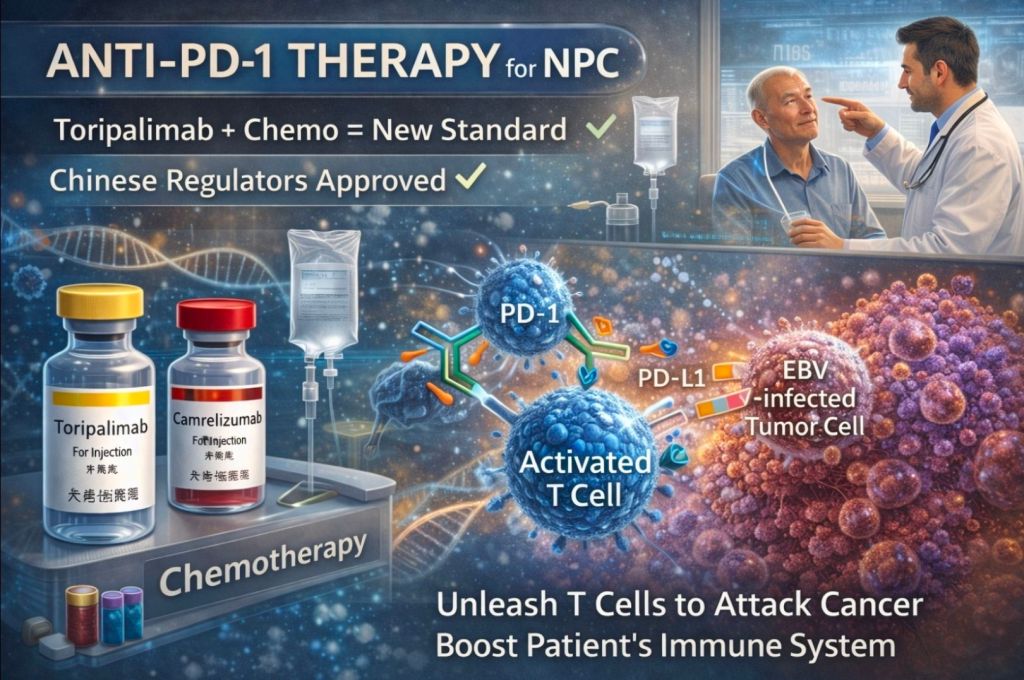
Even earlier in the course of disease, researchers are testing immunotherapy combos. Trials are adding a PD-1 blocker to induction chemo, or giving it as maintenance after chemoradiation. Early data are promising: some patients seem to have very durable remissions. Other experimental approaches include vaccines against EBV proteins. A few Phase I trials have tried vaccinating NPC patients with EBV antigens (like LMP2 or EBNA1) delivered by viral vectors or peptides. These aim to train the immune system to sniff out any remaining cancer cells. It’s still early, but imagine in the future giving a shot that baits and boosts immune cells against NPC – that would be a game-changer.

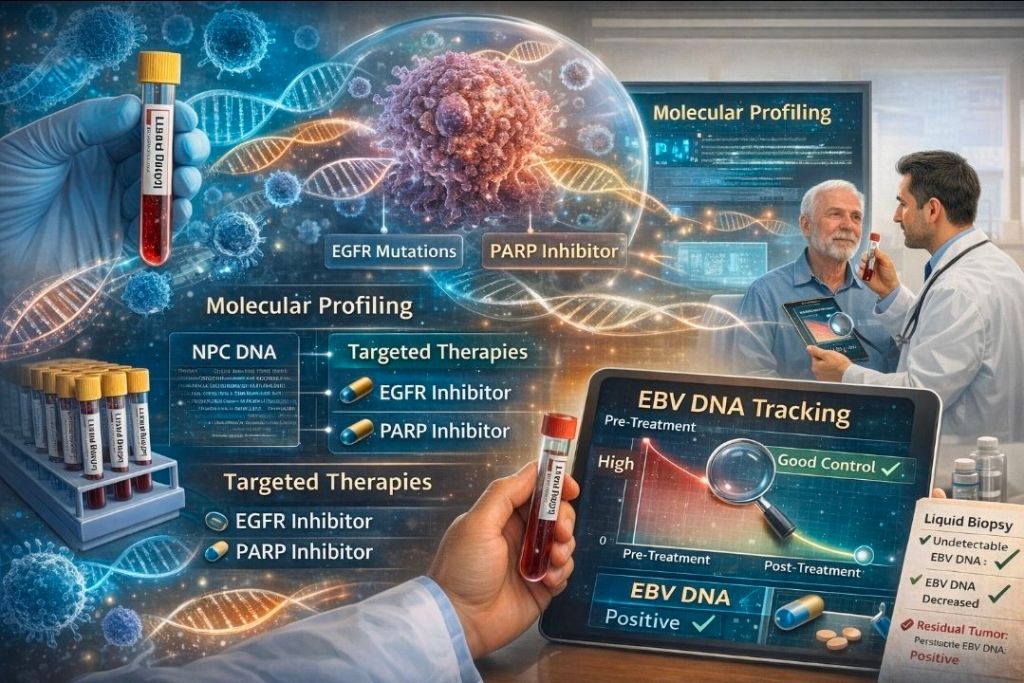
Beyond drugs, molecular profiling is growing. Scientists are sequencing NPC tumors to identify unique targets. For instance, some trials are exploring EGFR inhibitors or PARP inhibitors in select patients. Right now there’s no widely used targeted therapy (like there is for, say, EGFR-mutant lung cancer), but the research continues. The hope is to find any Achilles’ heel in NPC cells that’s druggable. Liquid biopsy (EBV DNA in blood) is another breakthrough: we can now track EBV DNA levels as a real-time marker. Before treatment, almost all NPC patients have detectable EBV DNA in blood. If the levels don’t go down after therapy, it often means residual tumor. Conversely, undetectable EBV DNA after treatment usually signals good control. This test feels like having a “CSI clue” in your bloodstream. Clinicians are using it more and more to personalize follow-up.
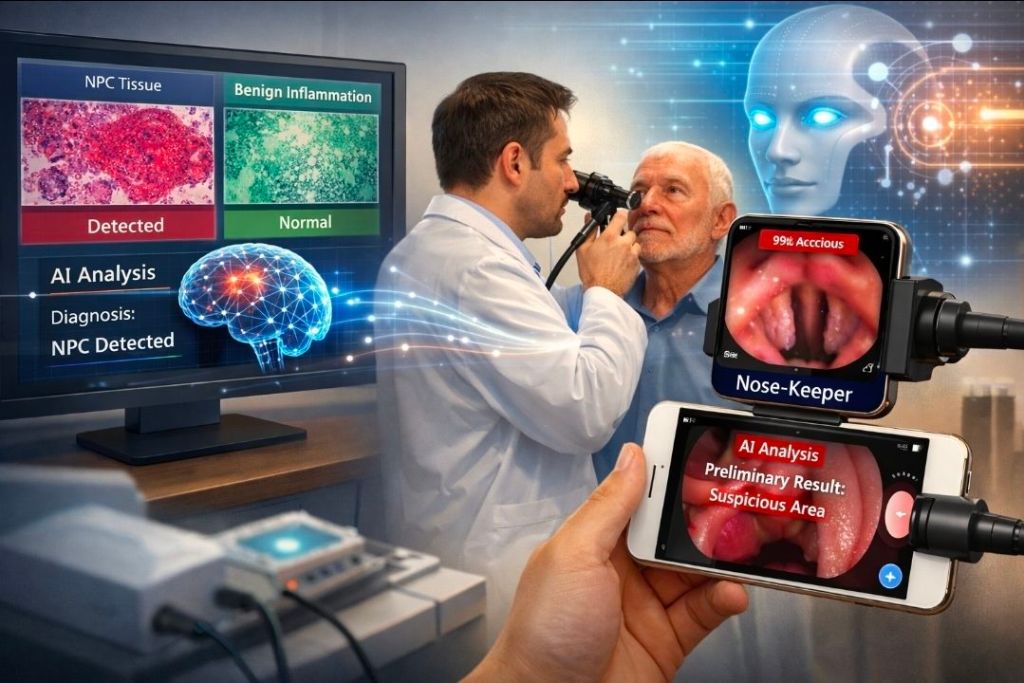
Lastly, high-tech tools are emerging. Artificial intelligence (AI) is already being trained to help doctors. Research teams have developed deep-learning models that analyze pathology slides or endoscopic images. For example, one AI model can distinguish NPC tissue from benign inflammation with remarkable accuracy. Another group created a smartphone app (“Nose-Keeper”) that assesses nasopharyngeal endoscopy images in real time. Reportedly, it had 96% sensitivity – almost like having an extra pair of (digital) eyes during exams. In the next few years, it’s conceivable you’ll bring AI to your check-up: maybe a phone adapter will take a quick nasal video and give the doctor a preliminary read.
In short, NPC research is vibrant. New clinical trials are everywhere, especially in Asia. There are even efforts to improve radiation delivery (proton therapy to spare more normal tissue), better supportive care, and psychosocial interventions for patients. We’re building an entire toolkit of advanced therapies, from vaccines and immuno-drugs to AI assistants and novel biomarkers. The science may sound like science fiction, but it’s steadily moving into real treatments.































Leave a comment