
Part 7: Prevention, Screening and Outlook
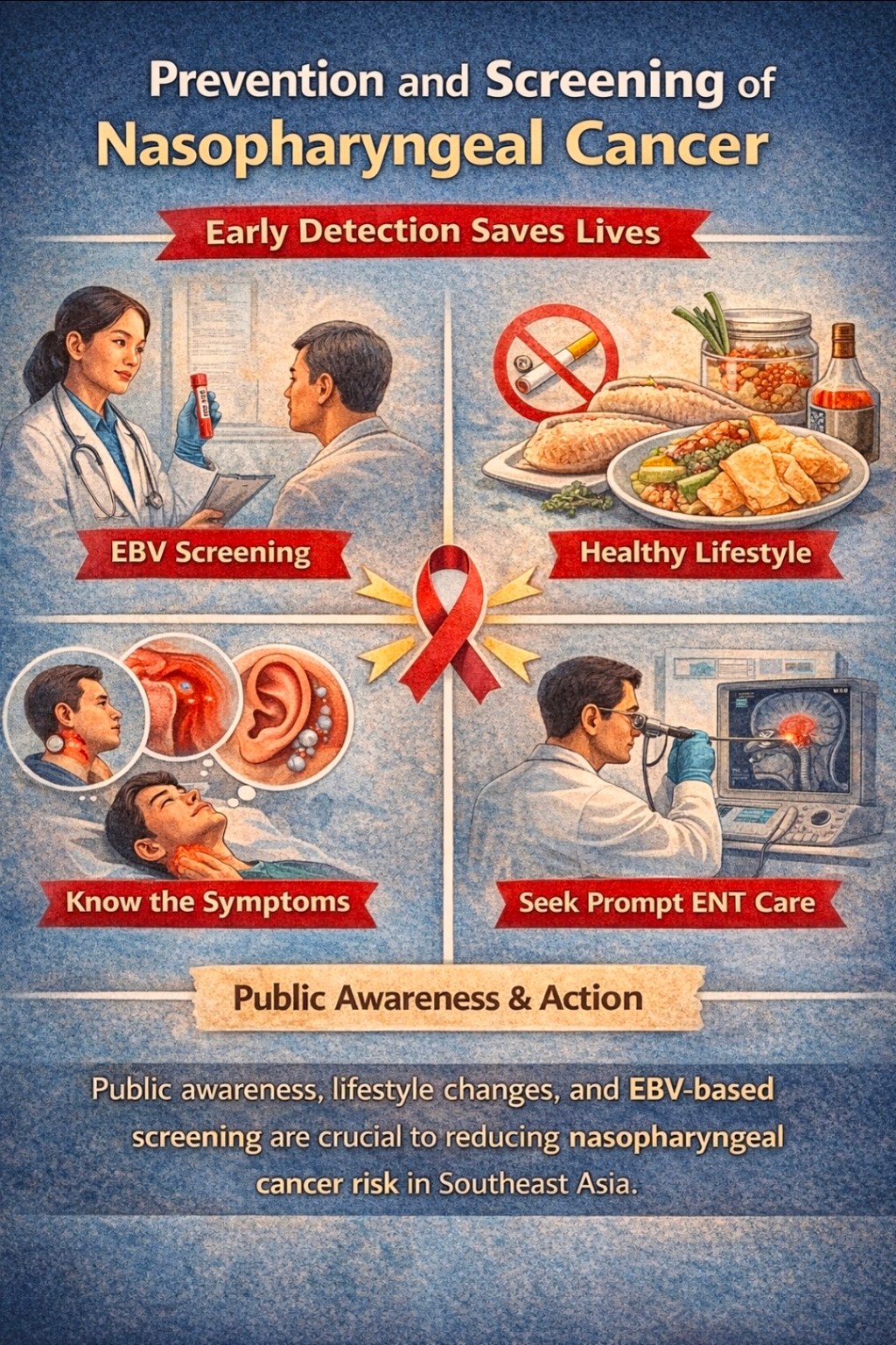
What does this all mean for patients and the public, especially in Southeast Asia? First, awareness is key. The chances of beating NPC are much higher when we catch it early. Doctors and health programs are increasingly promoting EBV-based screening in high-risk communities. For example, experts now recommend one or two rounds of screening for middle-aged adults (roughly ages 30–69) in Southern China and other very high-risk regions. This involves simple blood tests – either EBV antibody panels or plasma EBV DNA quantification. People with a family history of NPC (high-risk kin) in intermediate-risk areas (like parts of Southeast Asia) are also candidates for screening. Screening isn’t advised in low-risk populations (it would be cost-prohibitive and low-yield).

If a screening blood test is positive, the next step is prompt referral. That usually means an ear-nose-throat specialist will do the endoscopic exam and possibly an MRI. As noted earlier, MRI is a powerful tool: it can reveal small tumors that a scope might miss. In fact, adding a quick MRI to the workup barely increases the cost of care but can significantly improve early detection. Think of it like having both your eyes and ears for a search mission, rather than just your eyes.

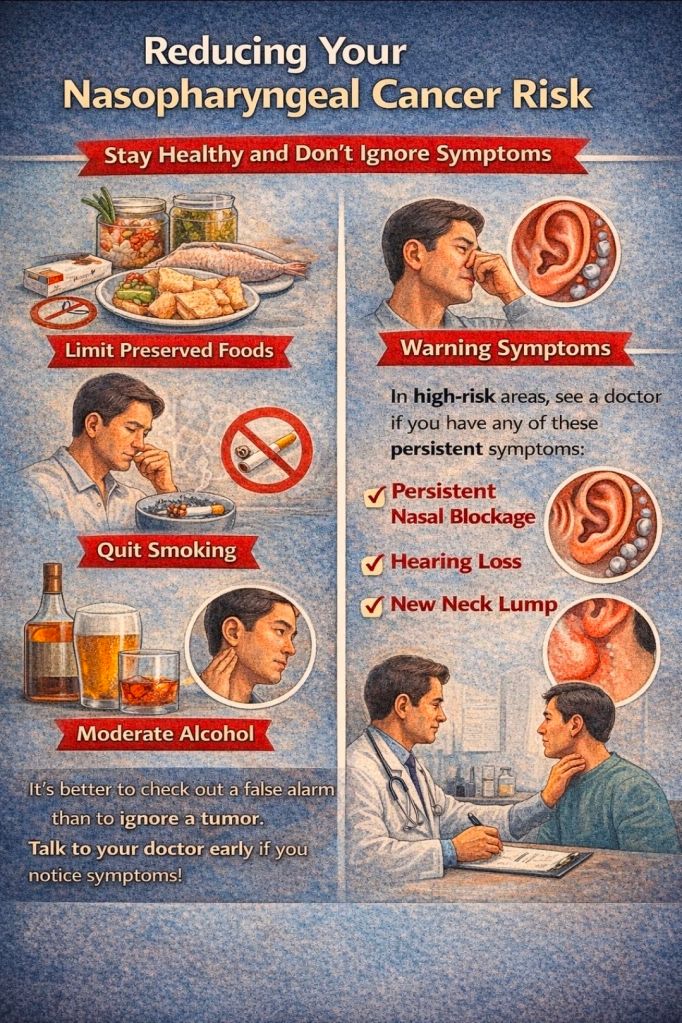
For individuals, reducing risk factors makes sense too. Limiting intake of heavily preserved foods, quitting smoking, and moderating alcohol are all reasonable preventive measures (even though NPC isn’t as straightforwardly tied to these as some other cancers are). Good general health and regular check-ups help too. And importantly: don’t ignore warning signs. In high-risk areas, anyone with a persistent one-sided nasal blockage, hearing loss, or a new neck mass should see a doctor and mention NPC. It’s better to evaluate a false alarm than to let a sneaky tumor grow.
Looking ahead, the battle against NPC is hopeful. Advanced radiation and chemo already allow many patients to be cured. The addition of immunotherapy and smarter drugs promises even higher cure rates for metastatic cases. Clinical trials on EBV vaccines and targeted therapies are ongoing. And with stronger screening programs (taking cues from models in China and Hong Kong), more cancers will be caught at stage I or II – where treatment can be swift and gentle.
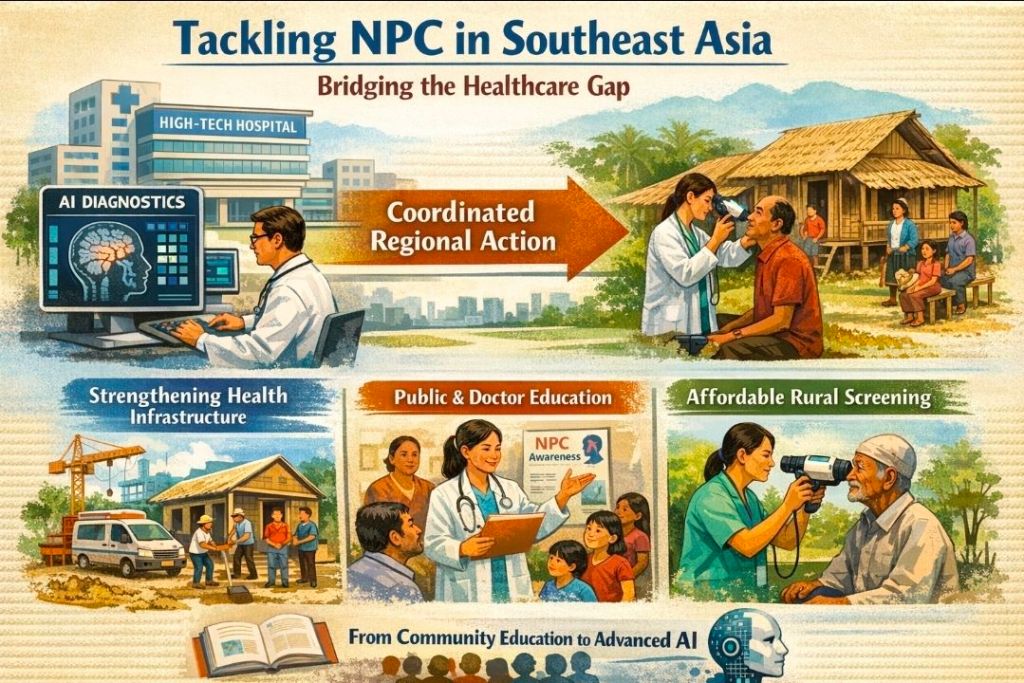
However, challenges remain. Southeast Asia has diverse healthcare systems, and not everyone has easy access to high-tech hospitals. As experts in a recent review stressed, coordinated regional action is crucial. This means strengthening health infrastructure, educating the public and doctors about NPC, and making screening affordable and available in rural communities. In short, we need to bring our best tools – from community education to high-end AI – to bear on this problem.
The good news is that NPC doesn’t have to be a mysterious death sentence. In countries like Singapore and Malaysia, where awareness and treatment are well-developed, 5-year survival is impressively high (often over 80% for early-stage cases). Even for late-stage, modern therapies are extending lives. If we keep pushing research, embrace innovation, and stay vigilant with screening, NPC can become a story of public health success rather than tragedy. After all, understanding its unique causes and behavior has already changed the game dramatically. With science on our side, that “Cantonese cancer” is losing its grip. Just like any foe we’ve studied carefully, it can be outsmarted and overcome – one patient at a time.































Leave a comment