PART 5: Diagnosis and Investigations of Tonsillitis
A Practical ENT Specialist’s Guide for Patients in Kuala Lumpur – by Dr Ameen
One of the most common things patients say to me is:
“Doctor, do I need a throat swab?”
The short answer? Not always.
The right answer? It depends — and that’s where ENT expertise matters.
Diagnosing tonsillitis isn’t just about shining a torch into the mouth and guessing. It’s a careful balance of clinical judgement, evidence-based guidelines, and individual patient factors.
Let me walk you through how tonsillitis is properly diagnosed in real-world ENT practice.
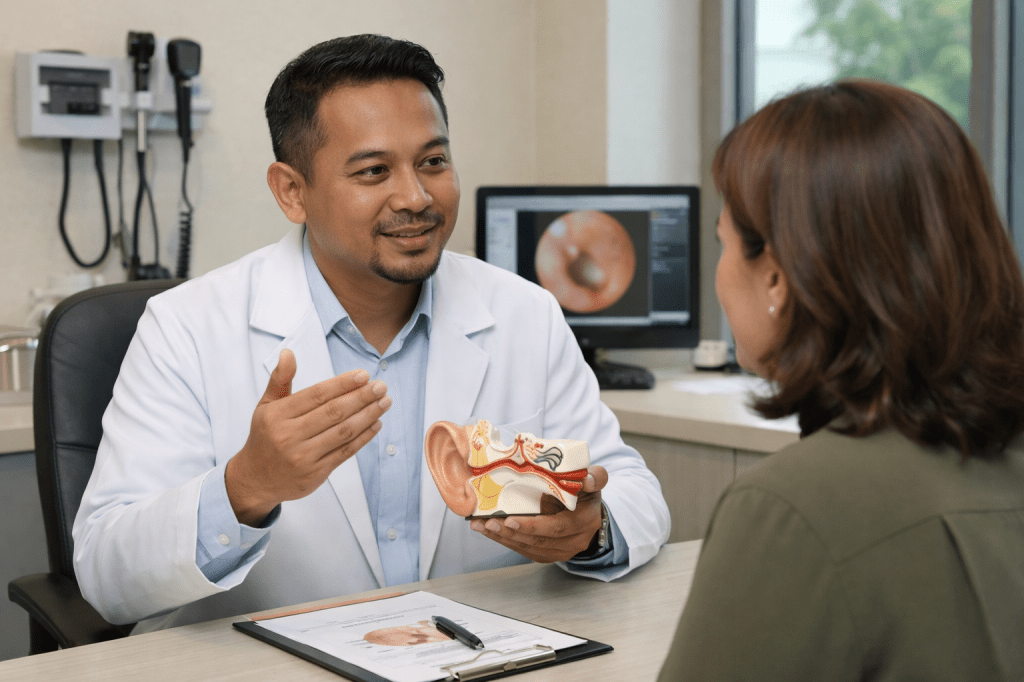
The Most Important Tool: A Detailed Clinical Assessment
Despite all our modern tests, clinical evaluation remains the cornerstone of tonsillitis diagnosis.
During an ENT consultation, I assess:
- Severity and duration of symptoms
- Presence of fever
- Swallowing difficulty
- Voice changes
- Neck swelling
- Previous episodes of tonsillitis
- Response to prior treatments
Medical evidence consistently shows that history and physical examination are often enough to determine whether tonsillitis is likely viral or bacterial.
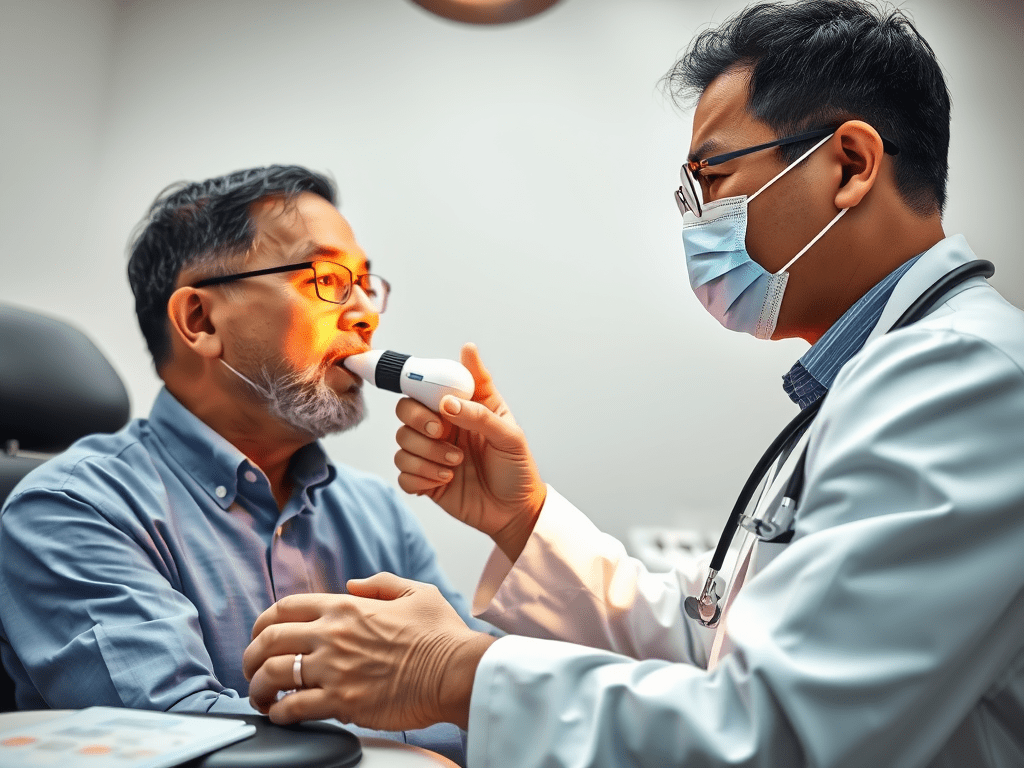
Throat Examination: What ENT Specialists Look For
Using proper lighting and instruments, an ENT specialist examines:
- Size and symmetry of the tonsils
- Colour (pink vs angry red)
- Presence of white or yellow exudates
- Signs of abscess formation
- Condition of surrounding throat tissues
Contrary to popular belief, white patches alone do not confirm bacterial infection. Viral tonsillitis can look equally dramatic.
This is why “Doctor Google” often misleads.
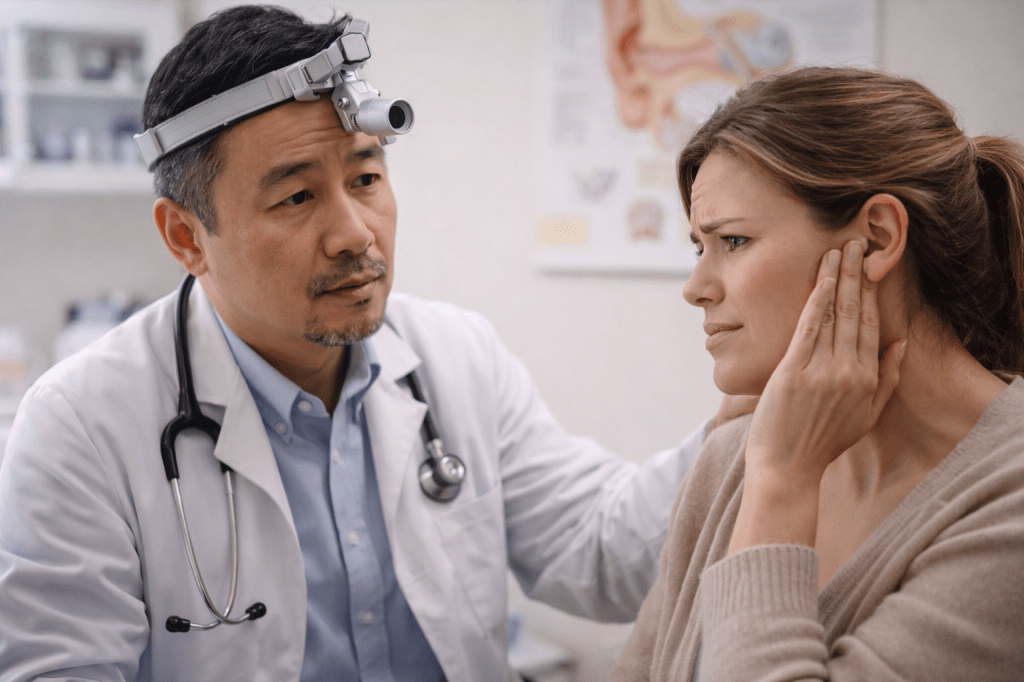
Neck Examination: The Clues Outside the Throat
The examination doesn’t stop at the mouth.
We also check:
- Cervical lymph nodes
- Tenderness or firmness
- Unilateral swelling
- Signs of deeper infection
This step is crucial for detecting complications such as peritonsillar abscess or deeper neck space infections.
Do You Always Need a Throat Swab?
This is where evidence-based medicine comes in.
Throat Swabs Are Considered When:
- Symptoms strongly suggest bacterial tonsillitis
- Fever is high and persistent
- There is no cough or runny nose
- There is concern for streptococcal infection
- Recurrent episodes raise diagnostic uncertainty
A throat swab helps detect Group A Streptococcus, guiding appropriate antibiotic use.
When Throat Swabs May Not Be Necessary
- Mild symptoms
- Clear viral features (cough, runny nose, hoarseness)
- Rapid improvement with supportive care
Unnecessary testing leads to unnecessary antibiotics — something we actively try to avoid in modern ENT practice.
Blood Tests: When Are They Needed?
Blood tests are not routine for simple tonsillitis.
They may be considered if:
- Symptoms are severe or prolonged
- Infectious mononucleosis is suspected
- There are systemic symptoms (extreme fatigue, liver enlargement)
- Complications are suspected
Tests may include:
- Full blood count
- Inflammatory markers
- Specific viral markers when indicated
Imaging: Rare but Sometimes Essential
Most tonsillitis cases do not require imaging.
However, ultrasound or CT scans may be ordered if:
- Peritonsillar abscess is suspected
- Neck swelling is asymmetrical
- There is difficulty opening the mouth
- Symptoms worsen despite treatment
These investigations help ENT specialists plan safe and effective treatment.
Why Accurate Diagnosis Matters
Misdiagnosis leads to:
- Repeated antibiotics
- Antibiotic resistance
- Delayed recovery
- Missed complications
- Unnecessary surgery fears
Accurate diagnosis, on the other hand, leads to:
- Faster recovery
- Targeted treatment
- Peace of mind
- Better long-term outcomes
In Kuala Lumpur, where patients often seek multiple opinions, a clear ENT-led diagnosis saves time, cost, and anxiety.
If you’re tired of repeated sore throats, conflicting advice, or unnecessary antibiotics, it’s time for clarity.
👉 Book an ENT consultation with me for an accurate diagnosis and evidence-based investigations tailored to your condition.































Leave a comment