PART 5: Diagnosis and Investigations for Neck Swelling
Neck swelling raises one big question.
👉 “Doctor, what tests do I need?”
The answer depends on how the swelling behaves, not just how it looks. Diagnosis of neck swelling follows a step-by-step approach. This avoids unnecessary tests while ensuring serious conditions are not missed.
As an ENT specialist, the goal is simple:
find the cause accurately and early.
Step 1: Detailed Medical History
Diagnosis always starts with a conversation.
Although it sounds simple, history-taking is powerful.
Key questions include:
- When did the swelling start?
- Has it changed in size?
- Is it painful or painless?
- Is it associated with infection?
- Are there voice, swallowing, or breathing changes?
- Is there weight loss or night sweats?
In addition, risk factors matter.
Smoking history, alcohol intake, and previous cancers guide urgency.
Therefore, never underestimate the importance of a proper consultation.
Step 2: Comprehensive Head and Neck Examination
Next comes physical examination.
This includes:
- Inspecting the neck visually
- Palpating the lump
- Assessing size, firmness, and mobility
- Checking surrounding structures
ENT specialists also examine:
- Mouth and throat
- Tonsils
- Tongue base
- Voice box
- Nose and nasopharynx
This full assessment is essential.
It allows localisation of the problem.

Step 3: Flexible Nasopharyngolaryngoscopy
Many patients worry about this test.
However, it is quick and well tolerated.
A flexible scope allows direct visualisation of:
- Nasopharynx
- Oropharynx
- Hypopharynx
- Larynx and vocal cords
This test helps detect:
- Hidden tumours
- Inflammation
- Structural abnormalities
Importantly, some cancers are not visible externally.
Scopes allow early detection.

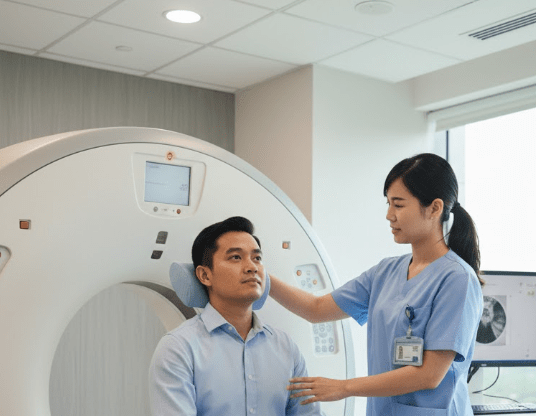
Step 4: Imaging Investigations
Imaging is chosen carefully.
Not everyone needs a scan.
Common imaging tests include:
Ultrasound of the Neck
This is often the first imaging choice.
It helps assess:
- Lymph nodes
- Thyroid nodules
- Salivary glands
- Cystic vs solid masses
Ultrasound is safe and radiation-free.

CT Scan (Computed Tomography)
CT scans are used when:
- Deeper structures are involved
- Cancer is suspected
- Surgical planning is needed
They provide excellent anatomical detail.
MRI Scan
MRI is useful for:
- Soft tissue characterisation
- Complex neck masses
- Certain salivary or skull base conditions
The choice depends on clinical findings.

Step 5: Tissue Diagnosis (Biopsy)
Imaging shows structure.
However, biopsy shows the truth.
Common biopsy methods include:
- Fine Needle Aspiration Cytology (FNAC)
- Core needle biopsy
- Open biopsy (selected cases)
FNAC is minimally invasive and widely used.
It helps differentiate benign from malignant causes.
Importantly, biopsy is only done when indicated.
Unnecessary procedures are avoided.
Step 6: Blood Tests and Additional Workup
Blood tests are supportive, not diagnostic alone.
They may include:
- Full blood count
- Thyroid function tests
- Inflammatory markers
- Infection screening
In selected cases, referral to:
- Endocrinology
- Oncology
- Infectious disease specialists
…may be needed.
This team-based approach ensures accuracy.
Why a Structured Approach Matters
Some patients request scans immediately.
However, skipping steps can cause confusion.
A structured diagnostic pathway:
- Reduces unnecessary testing
- Prevents missed diagnoses
- Shortens time to treatment
- Improves outcomes
Therefore, ENT-guided evaluation is crucial.
Common Patient Concerns
“Is investigation painful?”
Most tests are not painful.
“Do all neck lumps need biopsy?”
No. Many do not.
“Will tests delay treatment?”
On the contrary, proper diagnosis speeds it up.
👉 If you have persistent or unexplained neck swelling, proper investigation is essential. An ENT consultation in Kuala Lumpur ensures the right tests are done at the right time. Book an appointment for accurate diagnosis and peace of mind.
References
This article is written based on current evidence and clinical practice standards from leading ENT journals, including The Laryngoscope, JAMA Otolaryngology–Head & Neck Surgery, Otolaryngology–Head and Neck Surgery, Head & Neck, Clinical Otolaryngology, and European Archives of Oto-Rhino-Laryngology.
Reviewed by Dr Ameen, ENT Specialist, Kuala Lumpur
































Leave a comment